If you think keeping your low-density lipoprotein (LDL) cholesterol in check only matters for heart health, think again.
In August, the Lancet Standing Commission on Dementia Prevention, Intervention, and Care officially added high LDL cholesterol in mid-life as a modifiable risk factor for dementia. This expands their previous list of 12 risk factors and underscores the importance of recognizing and treating elevated LDL—especially for women.
Women often experience higher LDL after menopause and, despite this, are less likely to be prescribed cholesterol-lowering medications than men. The result: worse long-term outcomes for both heart and brain health.
Mind Over Matter® reviewed the science behind the Lancet Commission’s decision and spoke with leading experts to understand how high LDL contributes to dementia risk and what women can do to protect themselves.
Understanding LDL Cholesterol
Cholesterol is a waxy substance the body uses to build cell membranes, produce vitamin D, and create hormones. While your liver makes all the cholesterol you need, the rest comes from animal-based foods.
Cholesterol travels through your bloodstream via lipoproteins, which include:
-
LDL cholesterol (“bad cholesterol”) – carries fats to cells; needed, but harmful in excess.
-
HDL cholesterol (“good cholesterol”) – transports excess LDL back to the liver for removal.
Why Too Much LDL Is Dangerous
Excess LDL contributes to arterial plaque buildup, increasing your risk for:
-
Coronary artery disease
-
Cerebrovascular disease
-
Peripheral artery disease
-
Heart attack
-
Stroke
High LDL can result from genetics, aging, diets high in saturated/trans fats, refined sugars, obesity, smoking, diabetes, kidney disease, and certain medications.
How LDL Changes With Age
-
Girls have higher LDL than boys early in life.
-
Premenopausal women have lower LDL than men.
-
After age 50—around menopause—women experience a significant rise that surpasses men.
-
LDL levels decline in older age but more slowly in women.
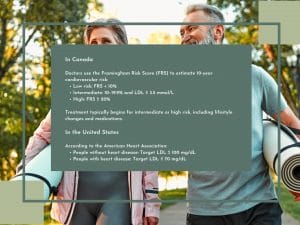
LDL Targets
Evidence Linking High LDL to Dementia
The Lancet Commission concluded that “high-quality, consistent, biologically plausible evidence exists that high LDL cholesterol in mid-life is a risk factor for dementia.”
Key supporting studies include:
-
+8% dementia risk for every 1 mmol/L increase in LDL in adults under 65 (UK, 1.1M adults).
-
33% higher dementia risk for LDL ≥ 3 mmol/L (PLOS One, 1.2M people).
-
5% higher all-cause dementia risk per 1 mmol/L LDL increase (UK databank, 1.8M people).
-
Risk was 10% higher in adults under 65.
-
How High LDL Raises Dementia Risk
Heart health and brain health are deeply connected. High LDL contributes to:
1. Vascular Disease
Atherosclerosis (arterial narrowing from plaque buildup) restricts blood flow. This can lead to:
-
Heart attack
-
Stroke
-
Vascular dementia — the second most common form of dementia
2. Chronic Inflammation
Inflammation plays a key role in both atherosclerosis and neurodegenerative disease.
Experts note that vascular disease and inflammation are major contributors to most forms of dementia, including Alzheimer’s, especially in Hispanic and African American populations.
Lowering LDL helps reduce vascular damage—one of the few modifiable dementia risks we can target today.
 Why Mid-Life LDL Matters for Women
Why Mid-Life LDL Matters for Women
“High LDL cholesterol is a proven cardiovascular risk factor,” says Dr. Christopher Labos, cardiologist and epidemiologist. “Anything that reduces cardiovascular disease and stroke also reduces vascular dementia risk.”
Dr. Betsy Mills of the Alzheimer’s Drug Discovery Foundation adds:
“Menopause seems to be a tipping point where the seeds of cardiovascular and dementia-related disease begin. It’s crucial for women to act in mid-life.”
How to Lower High LDL
The good news: many strategies help reduce LDL and support both heart and brain health.
Diet & Exercise
Harvard Medical School recommends:
1. Eliminate Trans Fats & Limit Saturated Fats
Avoid partially hydrogenated oils. Reduce red meat, high-fat dairy, butter, and shellfish.
2. Increase Healthy Fats
Choose polyunsaturated and monounsaturated fats from:
-
Olive, canola, sunflower oils
-
Nuts & seeds
-
Avocados
-
Fatty fish (salmon, trout, tuna, mackerel)
3. Eat Colourful Fruits & Vegetables
They provide fibre and natural cholesterol-blocking sterols/stanols.
4. Avoid Added Sugars & Refined Grains
Watch for sugar, corn syrup, and “-ose” ingredients. Prioritize whole grains.
Exercise Benefits
30–60 minutes of moderate-to-vigorous exercise daily can raise HDL (the “good” cholesterol) by 5–10%.
While exercise alone may not lower LDL significantly, it boosts the impact of a heart-healthy diet.
Realistically, diet and exercise typically lower LDL by 10–15%, as genetics drive most cholesterol production.
Medications to Lower LDL
1. Statins (first-line treatment)
Examples: atorvastatin, rosuvastatin, simvastatin. Benefits include:
-
Strong LDL reduction
-
Anti-inflammatory and antioxidant effects
-
20% lower all-cause dementia risk
-
32% lower Alzheimer’s risk
Side effects (rare): muscle soreness, temporary brain fog. Often resolved by switching medications.
2. Ezetimibe
Prevents cholesterol absorption in the liver; may be combined with statins.
3. PCSK9 Inhibitors
Injectables (Praluent®, Repatha®) that prevent LDL receptor breakdown. Very effective for stubbornly high LDL.
4. Bempedoic Acid (Nexletol® / Nexlizet®)
Oral non-statin option that reduces liver cholesterol production.
What Else…
-
High LDL cholesterol is one of the leading risk factors for heart disease and stroke in women, according to the Heart & Stroke Foundation of Canada.
-
You can set goals and track progress using the Women’s Brain Health Initiative’s BrainFit™ Mobile App, a habit tracker designed to help prolong cognitive vitality.
What Women Need to Keep in Mind
Dementia risk builds over decades. Mid-life LDL is a warning sign that vascular damage and inflammation may already be underway.
“High LDL is bad for everyone,” says Dr. Labos, “but women remain under-treated. More women need to recognize the risks and discuss treatment options with their doctors.”
Check out the original article in Vol 20 of Mind Over Matter